Introduction to Inomyalgia and Chronic Muscle Pain
Inomyalgia is a long-lasting muscle pain condition that has gained increasing attention in chronic pain discussions, yet it still remains under-recognized in routine clinical practice. The term itself is derived from “ino,” referring to muscle fibers or muscle tissue, and “myalgia,” which means muscle pain. Together, the word describes an ongoing state of muscular discomfort, soreness, tenderness, and low-grade inflammation that can interfere with daily functioning and overall well-being.
Although inomyalgia shares overlapping features with better-known conditions such as fibromyalgia, it is often described as having a more muscle-centered or inflammation-oriented presentation. This distinction has encouraged clinicians and researchers to explore inomyalgia as a potentially unique pain pattern rather than simply a variation of existing diagnoses. Unfortunately, because awareness is still developing, many individuals experience delayed diagnosis, incomplete explanations, or ineffective treatment plans.
This comprehensive guide is designed to serve as a topical cluster resource on inomyalgia. It explores what the condition is, why it occurs, how it presents, and how it can be managed effectively through medical care, lifestyle strategies, and emerging research. Whether you are a patient, caregiver, or health-conscious reader, this article aims to provide clarity, validation, and actionable insights.
What Is Inomyalgia?
Inomyalgia is best described as a chronic musculoskeletal pain disorder marked by persistent muscle aching, sensitivity, and stiffness that lasts for months or even years. Unlike acute muscle pain caused by injury or overuse, inomyalgia does not resolve easily with rest or standard pain relief methods.
The defining feature of inomyalgia is the involvement of muscle fibers and surrounding connective tissue. Many specialists believe the pain originates directly within the muscles themselves rather than being driven entirely by altered pain processing in the brain. This is one of the key factors that separates inomyalgia from more centralized pain syndromes.
Medical literature on inomyalgia is still evolving. Imaging scans and routine blood tests often appear normal, which can be frustrating for patients seeking answers. However, emerging research suggests that subtle inflammation, micro-injuries from repetitive strain, impaired muscle recovery, and abnormal pain signaling may all contribute to symptom development. Because of these nuances, some experts debate whether inomyalgia should be classified as a standalone condition or considered a subtype within the broader chronic pain spectrum.
Causes and Risk Factors of Inomyalgia
The development of inomyalgia is rarely linked to a single cause. Instead, it is thought to arise from a combination of biological, neurological, immune-related, and lifestyle factors that interact over time.
Biological and Neurological Contributors
One widely discussed mechanism is central sensitization. This occurs when the nervous system becomes overly reactive, amplifying pain signals even in response to mild stimuli. In people with inomyalgia, this heightened sensitivity can make normal muscle sensations feel painful or exhausting.
Another proposed factor is mitochondrial dysfunction. Mitochondria are responsible for producing energy within cells, and when they do not function efficiently, muscles may fatigue more quickly and recover more slowly. This may explain why deep fatigue often accompanies muscle pain in inomyalgia.
Hormonal imbalances can also influence symptoms. Chronic stress can disrupt cortisol levels and other hormones involved in inflammation regulation, pain perception, and immune response. Over time, this imbalance may intensify muscle soreness and prolong flare-ups.
Immune System and Inflammatory Factors
In some individuals, inomyalgia appears after viral or bacterial infections. These infections may trigger long-term immune activation or low-grade inflammation that persists even after the initial illness resolves. People with a family history of autoimmune disorders or chronic inflammatory conditions may be more vulnerable.
Although inomyalgia is not classified as an autoimmune disease, immune dysregulation is believed to play a supporting role in symptom persistence for certain patients.
Lifestyle and Environmental Triggers
Physical trauma, surgical recovery, repetitive strain injuries, and prolonged overexertion are commonly reported triggers. Occupations or hobbies that involve repetitive movements or poor ergonomics may place ongoing stress on muscle fibers, contributing to microtrauma and chronic soreness.
Emotional stress is another significant factor. Long-term psychological strain can worsen pain perception and reduce the body’s ability to heal, creating a feedback loop between stress and muscle pain.
Common Symptoms of Inomyalgia
Inomyalgia presents with a broad range of symptoms that can vary significantly between individuals. The intensity and pattern of symptoms may also fluctuate over time.
Persistent Muscle Pain and Tenderness
Ongoing muscle pain is the hallmark symptom. The discomfort may feel dull, aching, burning, or deeply sore. Some people experience localized pain in specific muscle groups, while others notice that the pain shifts from one area to another.
Tenderness is often present when pressure is applied to affected muscles. Physical activity, even at low intensity, can temporarily increase soreness.
Stiffness, Fatigue, and Weakness
Morning stiffness is common, with muscles feeling tight or heavy upon waking. This stiffness may ease gradually throughout the day but can return after periods of inactivity.
Fatigue is another defining feature. Unlike ordinary tiredness, this exhaustion is often disproportionate to activity levels and may persist despite adequate rest. Muscle weakness or a sense of reduced endurance can also occur.
Neurological and Sensory Symptoms
Many people report cognitive difficulties often referred to as brain fog. These may include trouble concentrating, forgetfulness, and slowed thinking.
Heightened sensitivity to cold temperatures, light touch, or pressure is frequently described. Muscle spasms or twitching may occur unexpectedly and can be painful.
Sleep and Mental Health Effects
Sleep disturbances are extremely common in inomyalgia. Individuals may struggle with insomnia, frequent awakenings, or unrefreshing sleep. Poor sleep quality can worsen pain, fatigue, and mood.
Over time, the burden of chronic symptoms may contribute to anxiety, low mood, or depression. These emotional responses are understandable and do not indicate weakness; rather, they reflect the complex interaction between chronic pain and mental health.
How Inomyalgia Is Diagnosed
Diagnosing inomyalgia can be challenging because there is no single test that definitively confirms the condition. Instead, diagnosis relies on careful evaluation and exclusion of other possible causes.
Clinical Assessment and Medical History
The diagnostic process usually begins with a detailed discussion of symptoms, including their onset, duration, triggers, and impact on daily life. A physical examination focuses on muscle tenderness, range of motion, and pain response.
Exclusion of Similar Conditions
Blood tests are often ordered to rule out inflammatory arthritis, autoimmune diseases, thyroid disorders, and metabolic imbalances. Imaging studies such as MRI may be used to exclude structural abnormalities, although they often appear normal in inomyalgia.
In rare cases, additional tests like muscle biopsies are performed if inflammatory muscle disease is suspected.
Specialist Involvement
Referral to specialists such as rheumatologists, neurologists, or pain management physicians is common. These professionals are more familiar with complex chronic pain patterns and can help distinguish inomyalgia from conditions with overlapping symptoms.
Inomyalgia vs. Fibromyalgia
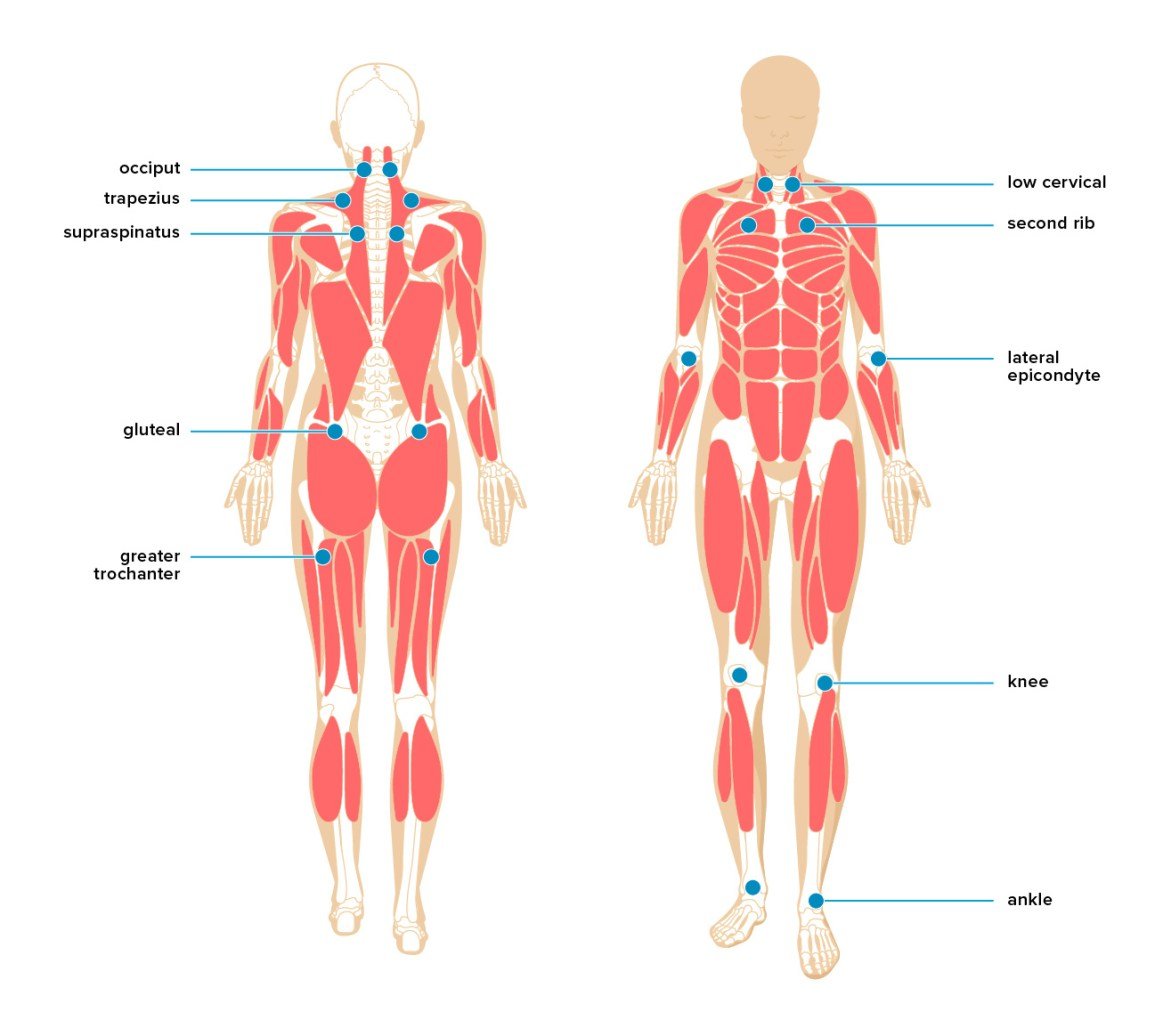
Inomyalgia and fibromyalgia are frequently compared because they share symptoms such as muscle pain, fatigue, and sleep disruption. However, important differences exist.
Inomyalgia often emphasizes localized or deep muscle involvement, whereas fibromyalgia is defined by widespread pain affecting multiple regions of the body. Fibromyalgia has established diagnostic criteria and is widely recognized in medical guidelines, while inomyalgia remains an emerging concept.
People with fibromyalgia frequently experience additional symptoms such as irritable bowel syndrome, migraines, and widespread tender points. In contrast, inomyalgia tends to focus more narrowly on musculoskeletal discomfort and muscle recovery issues.
The underlying mechanisms may also differ. Inomyalgia may involve peripheral muscle microtrauma and inflammation, while fibromyalgia is more strongly associated with central nervous system pain amplification.
Treatment Approaches for Inomyalgia
Managing inomyalgia typically requires a personalized, multi-layered approach that addresses pain, function, and overall health.
Medications and Medical Therapies
Nonsteroidal anti-inflammatory drugs may provide partial relief for some individuals, although results vary. Certain antidepressants, including duloxetine and amitriptyline, are sometimes prescribed to reduce pain sensitivity and improve sleep quality.
Medications originally developed for seizure disorders, such as gabapentin or pregabalin, can help calm overactive nerve signals. Muscle relaxants may be useful during periods of intense muscle tension or spasms.
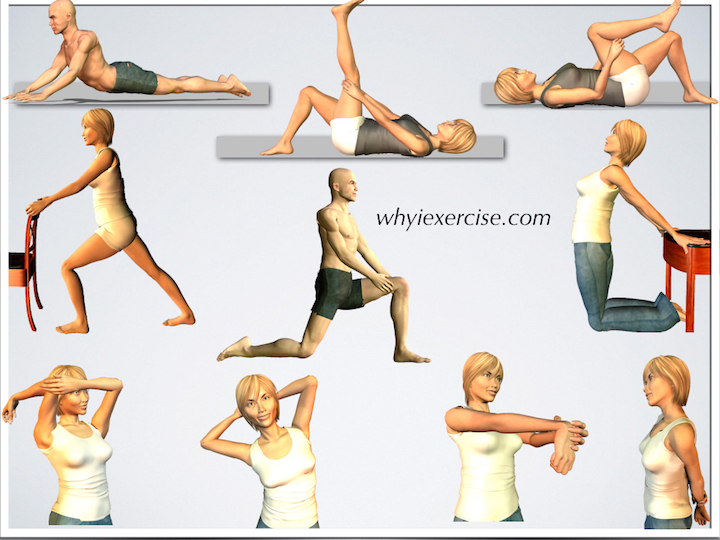
Physical Therapy and Movement-Based Care
Physical therapy plays a central role in long-term management. Gentle stretching, low-impact strengthening, and mobility exercises help maintain function without aggravating symptoms.
Activities such as swimming, water aerobics, yoga, and tai chi are often well tolerated because they reduce joint and muscle stress. Low-intensity use of equipment designed for controlled muscle engagement can also support stability and posture when used under professional guidance.
Complementary and Supportive Therapies
Cognitive behavioral therapy can help individuals develop coping strategies, reduce fear of movement, and manage the emotional effects of chronic pain. Massage therapy, acupuncture, and heat or cold applications may provide symptom relief for some patients.
Nutritional supplements, including magnesium, vitamin D, and omega-3 fatty acids, are sometimes recommended to support muscle health and reduce inflammation, but they should always be used with medical advice.
Role of Diet and Lifestyle in Inomyalgia Management
Lifestyle choices can significantly influence symptom severity and flare frequency in inomyalgia.
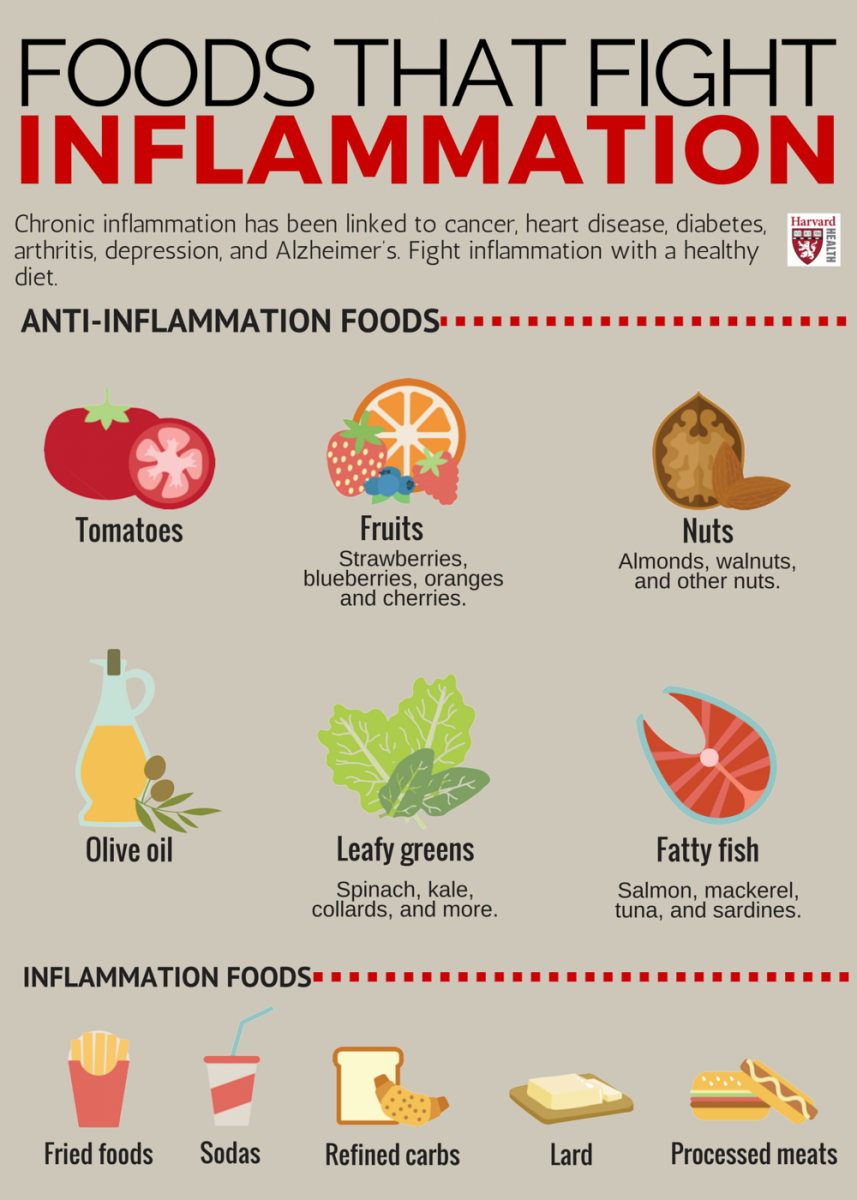
Anti-Inflammatory Nutrition
A diet focused on whole, nutrient-dense foods may help reduce muscle inflammation and support recovery. Emphasizing fruits, vegetables, lean proteins, healthy fats, nuts, seeds, and whole grains can provide essential nutrients.
Limiting processed foods, refined sugars, and excessive saturated fats may reduce inflammatory burden. Staying well hydrated is equally important for muscle function and energy levels.
Sleep and Stress Management
Restorative sleep is essential for muscle repair. Establishing a consistent sleep schedule, reducing evening screen exposure, and creating a cool, dark sleeping environment can improve sleep quality.
Stress reduction techniques such as meditation, deep breathing, and gentle movement practices help calm the nervous system. Learning to balance activity with rest is crucial to preventing overexertion and symptom flare-ups.
Emotional and Mental Health Considerations
The invisible nature of inomyalgia can make emotional coping particularly difficult. Many individuals feel misunderstood or dismissed, which can increase feelings of isolation.
Accessing mental health support is an important aspect of comprehensive care. Counseling, peer support groups, and online communities can provide validation and practical coping strategies. Keeping a symptom journal may also help individuals identify triggers and communicate more effectively with healthcare providers.
Daily Life Management Strategies
Living well with inomyalgia often requires thoughtful adjustments to daily routines. Pacing activities, using ergonomic tools, and incorporating regular rest breaks can help conserve energy.
Setting realistic goals and celebrating small accomplishments can foster a sense of control and progress. Consistency in nutrition, movement, and sleep routines supports long-term symptom stability.
Research and Future Directions in Inomyalgia
Research into inomyalgia is still developing, but interest in chronic muscle pain syndromes continues to grow. Future studies may focus on identifying biomarkers, understanding genetic susceptibility, and using advanced imaging to detect subtle muscle or nerve changes.
Innovations in molecular medicine and pain modulation therapies hold promise for more targeted treatments. Increased awareness and patient advocacy are likely to play key roles in advancing research and improving recognition within clinical practice.
Conclusion
Inomyalgia is a complex and often life-altering condition that affects muscles, energy levels, and overall quality of life. Although it is not yet as widely recognized as fibromyalgia, understanding of its unique features continues to improve. With early recognition, individualized treatment plans, and supportive lifestyle strategies, many people can achieve meaningful symptom relief and improved daily functioning. Ongoing research and advocacy offer hope for clearer diagnostic pathways and more effective therapies in the future.
FAQs About Inomyalgia
What is inomyalgia?
Inomyalgia is a chronic condition characterized by persistent muscle pain, tenderness, stiffness, and fatigue. The term combines references to muscle tissue and muscle pain and often emphasizes localized or inflammation-related discomfort.
What symptoms are most common in inomyalgia?
Common symptoms include ongoing muscle soreness, morning stiffness, fatigue, sensitivity to touch or cold, muscle spasms, sleep disturbances, and cognitive difficulties such as brain fog. Emotional effects like anxiety or low mood may also occur.
How do doctors diagnose inomyalgia?
Diagnosis involves a detailed medical history, physical examination, and ruling out other conditions through blood tests or imaging. There is no single diagnostic test, so clinical evaluation is essential.
Is inomyalgia the same as fibromyalgia?
No. While both involve chronic muscle pain and fatigue, fibromyalgia typically causes widespread pain and has established diagnostic criteria. Inomyalgia often focuses more on muscle-specific pain and localized inflammation.
What treatments help manage inomyalgia?
Treatment may include medications, physical therapy, gentle exercise, stress management, dietary changes, and supportive therapies such as counseling or supplements. A personalized, multi-approach plan is usually most effective.